What Is Gum Disease?
Gum Disease Explained
Many U.S. adults have some sort of gum disease, oftentimes without even knowing. Gum disease, also known as periodontal disease, is an infection of the surrounding tissue and bone that supports the teeth. This infection is caused by plaque bacteria that begins accumulating around the teeth and gum tissue. This build-up causes the gums to become red and inflamed.
If the plaque is not removed with daily brushing and flossing, the bacteria can damage not only your gums and teeth but as well as the supporting bone. This can lead to teeth becoming loose, falling out, or eventually requiring extraction by a professional.
Gum disease ranges from simple gum inflammation, known as gingivitis, to severe damage to the gums and supporting bone that is experienced in the advanced stage of periodontal disease, known as advanced periodontitis. Whatever the case, our specialists are knowledgeable and experienced in treating any form of gum disease.
Healthy Gum Tissue
Normal, healthy gum tissue appears to have a firm and coral-pink color. In addition, healthy gum tissue securely and tightly hugs the teeth. No redness is also present near the gumline where the gum tissue meets the teeth. While brushing, flossing, or eating certain foods, the gums will remain pink and firm without any bleeding or swelling.
It is vital to remember that healthy gums are not only beneficial for your oral health, but they significantly affect your overall health as well. Extensive research studies have been made that suggest the correlation between periodontitis and chronic severe health conditions, such as heart disease and diabetes.
Stages of Gum Disease
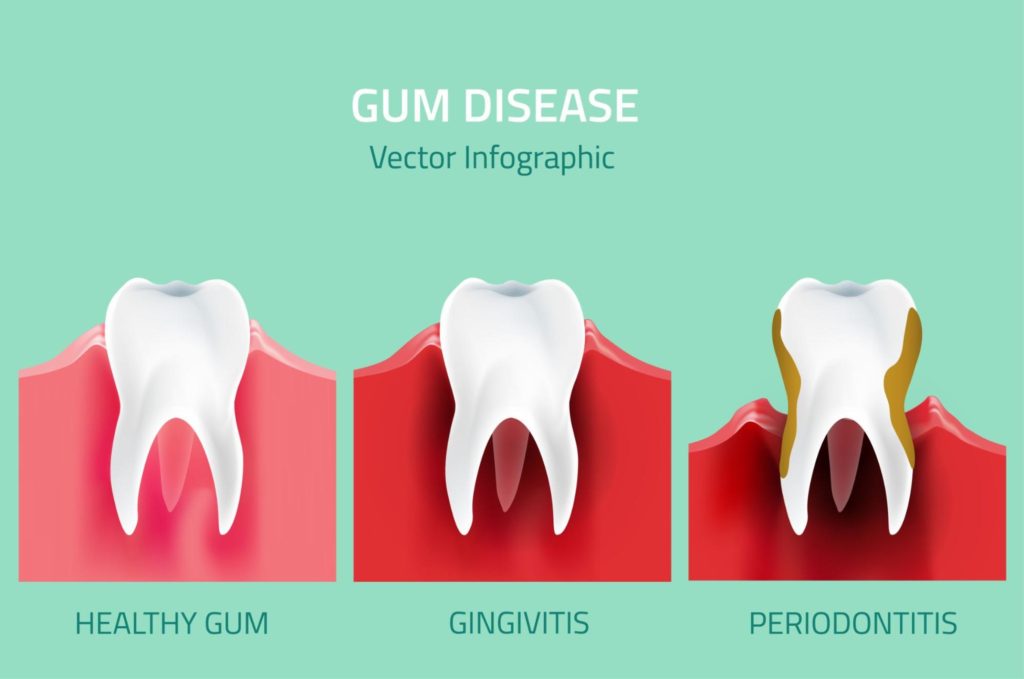
Gingivitis
Gingivitis is the very early stage of gum disease. During this stage, the gums and surrounding tissue are inflamed and sensitive. Although the gums are irritated during this stage, the teeth are still firmly stable in their sockets. The damage caused by gingivitis can also be reversed with proper oral hygiene maintenance and regular dental checkups. Common symptoms of gingivitis include:
- Bleeding while brushing or during probing
- Possible bad breath and/or a bad taste in the mouth
Mild Periodontitis
Mild periodontitis is a slightly more severe form of gingivitis. During this phase, there is more pronounced gingival bleeding and swelling. The gum tissue may begin to pull away from the teeth, forming small pockets. Pockets collect any food particles and debris which can cause infections. Symptoms of mild periodontitis include:
- Bad breath and/or a bad taste in the mouth
- Pockets measure 3-4 millimeters deep
Moderate Periodontitis
When gingivitis is left untreated, it can progress to moderate periodontitis. During this stage of gum disease, the gum layer attached to the teeth begins to pull away, forming slightly deeper pockets, which can cause moderate bone loss. The pockets can measure between 4-6 millimeters deep, and teeth tend to look longer due to gum recession. Other symptoms include:
- Gum boils or abscesses may develop
- Possible bad breath and/or a bad taste in the mouth
- Teeth may begin to drift and show spaces
Advanced Periodontitis
is the most severe stage of gum disease. The pocket size is now 6 millimeters or more profound, and there is severe bone loss. Due to the enlarged pocket depth and bone loss, teeth may become loose or mobile. This will affect the bite alignment; teeth may have to be extracted if treatment is ineffective. Other symptoms of advanced periodontitis include:
- Constant bad breath and/or a bad taste in mouth
- Teeth sensitivity due to exposed roots
Treatment Options for Gum Disease
The early stages of gum disease can often be treated and reversed by practicing proper brushing and flossing techniques. Maintaining proper oral hygiene will help prevent any future plaque build-up. The only effective way to remove tartar (plaque that has built up and hardened) is with a professional dental cleaning. For more severe cases of gum disease, such as advanced periodontitis, scaling and root planing are recommended to effectively remove the plaque and tartar that has grown below the gumline. Scaling helps remove the plaque above and below the gum line, while root planing is performed to smooth any irregularities on the teeth roots.
Scaling and Root Planing
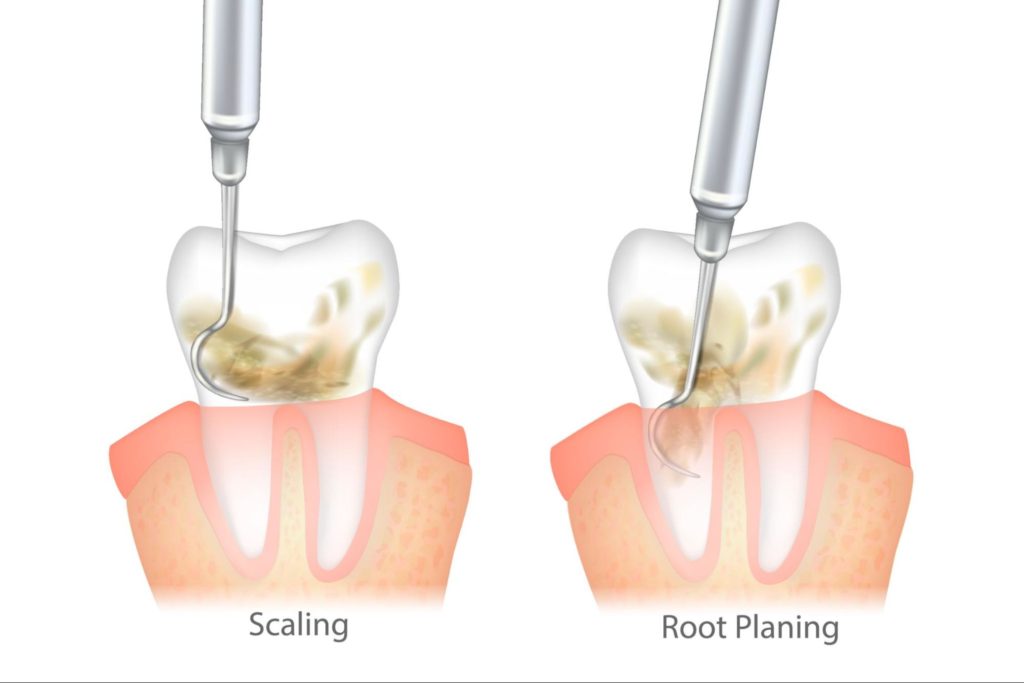
Periodontal scaling and root planing are standard procedures used to treat gum disease. It is a non-surgical, deep dental cleaning that is performed below the gumline. The main goal of this procedure is to remove any plaque or tartar that accumulates below the gum line and onto the tooth’s root. If the plaque or tartar is not removed, it can lead to more serious complications, such as bone deterioration, which can lead to loose teeth or, eventually, complete tooth loss.
This procedure involves two parts: scaling and root planing. Before the periodontal scaling and root planing are performed, our specialists administer a topical or local anesthetic to numb the area. Dental scaling involves the removal of the plaque and tartar, yellow or brown hardened plaque, and deposits on the tooth surface above and below the gum line.
Dental root planing is the smoothing of the root surfaces in order to promote the reattachment of the gum tissue to the tooth. During this part of the procedure, our specialists will smooth the rough surfaces of the tooth root to provide a healthy surface for healing.
Depending on the severity of the case, periodontal scaling and root planing may take more than one visit to treat the gum disease fully. Our specialists take the time to fully assess every patient to ensure they receive the quality dental care they deserve.
LANAP Therapy
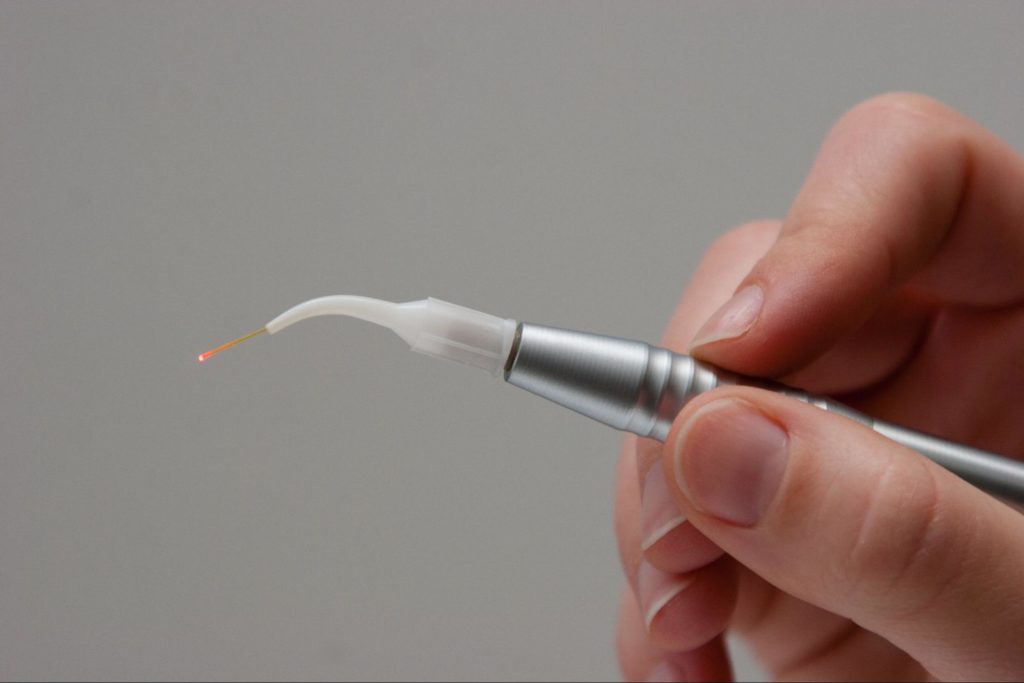
Another effective form of periodontal or gum disease treatment is known as LANAP therapy treatment. LANAP therapy is an innovative and minimally invasive treatment option for gum disease. With LANAP, you can visit our experienced Periodontists, receive treatment, and perform your regular day-to-day activities instantly.
With Laser assisted new attachment procedure (LANAP) therapy, our trained specialists utilize a laser tool to target and remove any diseased tissue that has been affected by gum disease. There are no sharp tools or scalpels needed for this procedure. Therefore, there is no need to worry about painfully removing the tissue. LANAP is minimally invasive and has a much faster healing time compared to traditional gum surgeries.
Before performing the LANAP procedure, our Periodontists will fully examine the severity of the gum disease by probing the periodontal pockets to determine the level of treatment needed for each tooth. Once examined, we then use a fine laser tool to eradicate the affected gum tissue. Dental scalers and other tools may then be used to remove the disease-causing plaque and tartar.
The laser stimulates healthy gum tissue to provide new healthy attachments and improve the overall healing rate of the gum tissue.
Osseous Therapy

Osseous therapy is a treatment option that is recommended for patients with advanced periodontitis. It is a procedure that allows our Periodontists to gain access to the root of the tooth for the removal of plaque, calculus, and diseased tissue. The main goal of this procedure is to reduce the formation of deep periodontal pockets formed by periodontal disease.
Our specialists first administer a local anesthetic. Once the area is numbed, our Periodontist will make a small incision along the gumline of the affected area. This incision will expose the tooth root’s surface, allowing our Periodontists to remove the disease-causing bacteria. Following the removal of the bacteria, we will smooth down any irregular areas that require reshaping due to the effects of gum disease. The gum tissue is then carefully sutured back into place. Flap therapy may sometimes be accompanied by minor osseous (bone) shaping or removal to ease tissue positioning, facilitate home care, and simplify maintenance appointments.
Guided Tissue Regeneration

Guided tissue regeneration (GTR) is a regenerative technique that aims to repair periodontal defects so that the tooth or set of teeth has more stability and support. This procedure involves using a biocompatible membrane material, often combined with a bone graft, that promotes the growth of lost tissue and bone around the tooth’s surface. This biocompatible membrane is vital as it prevents the faster migrating soft tissue cells from growing into the site and allows the slower migrating bone-producing cells to produce there instead.
To prevent pain or discomfort during the guided tissue regeneration (GTR) procedure, we will first administer local anesthesia to numb the area. A procedure known as a flap is then performed to open the gums and expose the roots and the bone. This area is then cleaned, and all bacteria deposits are removed. The biocompatible membrane is then placed over the damaged bone before closing the gum tissue back into place.
The membrane provides the necessary space and time for the bone to heal and begin to regenerate itself properly. Not every patient case is suitable for grafting. That is why our specialists will carefully and thoroughly examine every patient to ensure proper treatment is given.
Gum Disease Risk Factors
Periodontal diseases are bacterial infections or diseases which affect the gums. This disease can lead to gingivitis (inflammation of the gums at its earliest stage) and periodontitis (a more severe disease affecting the gum teeth, dental bone, and other periodontal tissues).
Gum disease can affect anyone. Symptoms can appear when there is no association between risk factors. Dental plaque is triggered by brushing and flossing. Your chances of gum disease are high in the presence of dental plaque and other gum disease risk factors listed below.
The Most Common Periodontitis Risk Factors
From genetic to environmental factors, below are some of the most common risk factors for gum disease:
- Inadequate oral hygiene
- Tobacco smoking
- Genetics
- Stress
- Diabetes
- Obesity
- Oral Piercings
Inadequate Oral Hygiene

Poor oral hygiene is one of the environmental risk factors for periodontal disease, and it’s simple to understand why. Bacterial deposits (biofilm, plaque) regularly form on the surfaces of the teeth.
If you do not maintain proper oral hygiene, gum disease will increase. Removing dental plaque and tartar periodically and thoroughly with the appropriate tooth-brushing and flossing products is essential in preventing gum disease.
What To Do
It is vital to clean your teeth and the spaces between your teeth and gums thoroughly at least twice a day with a toothbrush, interdental brush, and appropriate toothpaste.
Smooth tooth surfaces prevent plaque from re-accumulating. Ensure that your toothpaste has fluoride, sodium lauryl sulfate, potassium nitrate, and/or calcium carbonate, preferably as the active ingredient. You can also use mouthwash solutions if advised by a dental professional.
Tobacco Smoking

Smoking has, without any possible doubt, significant repercussions on the oral mucous membranes and, more particularly, on the periodontium. According to the Dental Investigation Society, tobacco masks gingival inflammation. The smoker’s gums will bleed less when brushing and will not alarm the patient about their periodontal condition.
Tobacco smoking, therefore, plays a determining role in the development of periodontitis. Amplifying the bone deterioration process increases periodontitis’s prevalence and severity and decreases the effectiveness of periodontal disease treatments.
Tobacco acts on the immune system, the blood vessels, and the oral environment: it disrupts the bacterial flora, increases the oral temperature, and modifies saliva flow.
Smokers generally have a higher quantity of tartar, more significant bone destruction, even if the clinical signs of inflammation are most often masked, and poorer healing after periodontal treatment, whether surgical or not. Finally, tobacco increases the risk of recurrence.
Precautions To Take
Smoking cessation is vital in periodontal management. This also offers an improvement in general health, a reduction in the risk of periodontitis, and a reduction in other oral pathologies such as oral cancer.
Genetics
Regarding the genetic risk factors for periodontal disease, the periodontium of patients and vulnerability to dental plaque are different. This is partly explained by genetic susceptibility to periodontal destruction, which varies from individual to individual. It is essential to learn about the periodontal situation of one’s family history.
The Evidence
The first evidence is a higher risk of developing periodontal disease when one of the parents or siblings is affected. This concept is called “family aggregation,” meaning that certain families present more often or more severely with periodontal disease.
Several research teams have studied families affected by severe forms of periodontal disease over several generations. Some studies have looked at the diseases in twins and compared identical and fraternal twins to identical twins who did not grow up together. Identical twins share the same genetic heritage since they come from the same oocyte and sperm, unlike fraternal twins, which come from two different sperm.
These studies show that the state of periodontal health, good or bad, is very similar in identical twins, whether they are raised in the same environment or not. This level of similarity is higher than that of fraternal twins.
How Genetics Also Helps Manage Periodontal Diseases
Genetics is a formidable prevention tool. With it, individuals who are at risk of developing periodontitis before they show symptoms of the disease are identified. Therefore, Periodontists and patients try to prevent its onset through routine check-ups or special attention to oral hygiene.
Then, in affected patients, genetic tests can help determine the prognosis of the remaining teeth and guide the choice of this or that treatment. Finally, the possible identification of genes associated with periodontitis could help in understanding these diseases and in the development of new biological therapies.
Stress
Stress is the process involving an external event that affects an individual’s normal balance of bodily functions. There are many ways to react to stress, and they can be classified into two main families: passive responses and active responses. These vary according to individuals and situations. Stress-related problems begin when the response to the stressor is inadequate, either in intensity or duration.
Stress acts in two groups on the periodontal level: behavioral and biological. Stress weakens the immune system and the response to infections, influencing the onset of progressions of periodontal disease.
- Behavioral Action. This can lead to a change in lifestyle habits by favoring those known to be harmful to periodontal health: poorer oral hygiene, tobacco use, consumption of alcohol or drugs, poor eating habits, reduction in the frequency of dental visits, and more.
- Biological Action. This also acts directly at the cellular level by activating several biological phenomena to reduce the action of the immune system and promote tissue deterioration.
The Evidence
Stress has been identified as a predisposing factor in necrotizing ulcerative gingivitis. This particular type of periodontal disease results in sharp and spontaneous pain requiring rapid treatment but healing quickly.
Several studies have since been carried out to define the role of stress on gingivitis and periodontitis. Most agree that stress is a risk factor for periodontal disease. This finding is all the more true for aggressive, rapidly evolving periodontitis and individuals with passive coping.
In stressed individuals, there is an increase in the prevalence of periodontitis due to a greater susceptibility to infection. Their periodontitis will evolve faster, and their response to treatment will be delayed. Do not hesitate to tell your dental professional or Periodontist about stressful elements in your life, acute or chronic.
Diabetes
The connection between diabetes and periodontitis has now been demonstrated. Uncontrolled diabetes can influence the onset or progression of periodontal disease. Periodontitis is considered the 6th complication of diabetes. Similarly, some studies show that active periodontitis could disrupt the stabilization of diabetes. Therefore, it is necessary to act on both pathologies simultaneously.
Diabetes is characterized by an abnormally high level of glucose in the blood. This hyperglycemia is due to a deficiency in the secretion of a hormone called insulin. This hormone stimulates glucose storage in liver cells, reducing glucose concentration in the blood.
For diabetic patients, either the pancreatic cells responsible for insulin secretion are dysfunctional (Type I), or there is resistance from insulin-sensitive cells in the liver, muscle, or a combination of both (Type II).
How Is Diabetes One Of The Most Common Periodontitis Risk Factors?
Diabetes will limit the functioning of defense cells, facilitating bacterial persistence in the periodontal pocket and increasing periodontal deterioration.
It is now established that diabetes is a risk factor for the appearance of gingivitis and periodontitis. In an epidemiological study conducted in the United States and presented by the Centres for Disease Control and Prevention (CDC), adults with poorly controlled diabetes were 2.9 times more likely to have periodontitis than non-diabetics. Conversely, people with well-controlled diabetes present a risk of periodontitis similar to non-diabetic patients.
Obesity

Obesity is one of the systemic factors of periodontal disease. Since 1997, obesity has been recognized by the WHO as a chronic disease due to an abnormal or excessive accumulation of body fat which represents a health risk.
The Observation
Numerous studies have shown an increased periodontal risk in obese patients, and even more susceptible are young adults. It also seems that being overweight, obese, weight gain, or an increase in waist circumference can increase the periodontal risk.
The Hypotheses
The biological mechanisms of this association are not clearly identified. However, being overweight and obese modify the characteristics of the inflammatory reaction, which is a significant component of periodontal disease. In this way, obesity could increase the risk of periodontitis.
The Results
In overweight or obese people, screening for periodontal disease should be systematized. This screening is more interesting since the response to periodontal treatment is not hampered compared to patients whose BMI is within the norm.
Oral Piercings
Oral piercings belong to the family of local risk factors. They deteriorate the tooth’s supporting tissues when they come into contact with them. Most of the risk factors of periodontitis are known as general risk factors because their influence exceeds the environment of teeth.
These piercings are done mostly by the young adult population (15-30 years old), mainly women. The most common location is the tongue, followed by the lip.
The Risk
During the installation, the main complication is pain. There are also cases of bleeding, infection, or exacerbated inflammatory reaction. However, other complications may appear over time. These are mainly gingival recessions and teeth fractures close to the piercing.
Tongue piercings cause more problems than lip piercings, especially when the bar is extended. In addition, piercings are “nests for bacteria.”
The Precautions To Take
To limit these complications, it is essential to:
- Regularly remove and clean the piercings
- Only use silicone closures
- Get frequent check-ups with your dentist
When periodontal diseases appear, they develop faster. They will be more challenging to deal with in the presence of dental plaque and risk factors such as tobacco, uncontrolled diabetes, susceptibility linked to genetics (heredity), stress, and more.
Identifying these risk factors makes it possible to prevent the development of periodontal disease. Also, controlling them is essential for the conduct of periodontal treatment.
FAQ
What is gum disease?
Gum disease develops when the bacteria found in plaque begin to build up around the teeth and gums. This build-up causes the gums to become red and inflamed. If the plaque is not removed with daily brushing and flossing, the bacteria can damage not only your gums and teeth but as well as the supporting bone.
What are dental scaling and root planing?
Periodontal scaling and root planing are common procedures used to treat gum disease. It is a non-surgical, deep dental cleaning that is performed below the gumline. The main goal of this procedure is to remove any plaque or tartar that accumulates below the gum line and onto the tooth’s root. If the plaque or tartar is not removed, it can lead to more serious complications, such as bone deterioration, which can lead to loose teeth or, eventually, complete tooth loss.
What is LANAP therapy?
LANAP therapy is an innovative and minimally invasive treatment option for gum disease. With Laser assisted new attachment procedure (LANAP) therapy, our trained specialists utilize a laser tool to target and remove any diseased tissue that has been affected by gum disease. There are no sharp tools or scalpels needed for this procedure.
What is osseous therapy?
Osseous therapy is a treatment option that is recommended for patients with advanced periodontitis. It is a procedure that allows our Periodontists to gain access to the root of the tooth for the removal of plaque, calculus, and diseased tissue. The main goal of this procedure is to reduce the formation of deep periodontal pockets formed by periodontal disease.
What is guided tissue regeneration (GTR) therapy?
Guided tissue regeneration (GTR) is a regenerative technique that aims to repair periodontal defects so that the tooth or set of teeth has more stability and support. This procedure involves using a biocompatible membrane material, often combined with a bone graft, that promotes the growth of lost tissue and bone around the tooth’s surface. This biocompatible membrane is vital as it prevents the faster migrating soft tissue cells from growing into the site and allows the slower migrating bone-producing cells to produce there instead.
What are the stages of gum disease?
The stages of gum disease include:
- Gingivitis. This is the earliest stage of periodontal disease, where the gums are inflamed due to bacterial build-up along the gumline. The damage occurring at this stage can be reversed since the supporting bone and tissue have not been compromised.
- Periodontitis. During this stage of periodontal disease, the supporting bone and tissue are now irreversibly damaged. The bacteria has progressed below the gum line, and your gums may form pockets that trap food and plaque.
- Advanced Periodontitis. This is the most advanced and severe stage of periodontal disease. During this stage, the supporting bone and tissue are destroyed, which causes teeth to shift, drift, or eventually fall out.
Who is most at risk for gum disease?
A smoker, an obese person, and those who ignore oral hygiene risk gum disease. Also, age is a risk factor for gum disease. According to the CDC data, 70% of people 65 years and older have some type of gum disease.
What are the leading causes of gum?
The leading causes of gum disease are dental plaque and tartar formation. Not correctly brushing and flossing can cause small bacteria buildup in the form of a sticky white film on the teeth or in the junction between the tooth and gum. Gum disease may affect you if this combines with one or two risk factors.
What three risk factors may make someone more likely to develop gum disease?
The three most common risk factors for gum disease include inadequate oral hygiene, tobacco smoking, and diabetes.
What is the local risk factor for periodontal disease?
One of the local risk factors is oral piercings. It can damage the tooth’s supporting tissues when they come into contact with them. Then as the piercings nest bacteria, gum diseases may occur. Other local risk factors for periodontal diseases include injury or damage to the gum, tooth position, carries, and more.
How long can you keep your teeth with periodontal disease?
If gingivitis is left untreated, it can lead to severe periodontitis and become more noticeable in a matter of weeks. Depending on the risk factors, periodontitis may lead to pain and tooth or periodontal tissue deterioration in a couple of months or a few years. It would only be best resolved with extraction and/or surgery.

